Trigeminal Neuralgia
What is Trigeminal Neuralgia?
Microvascular Decompression is one type of surgical treatment for intractable Trigeminal Neuralgia.
Trigeminal Neuralgia is a clinical diagnosis characterized by paroxysmal attacks of pain usually lasting less than two minutes. The pain is sudden and intense. It is usually described as sharp, stabbing, electrical or like “lightening striking” and is distributed along one or more of the divisions of the trigeminal nerve.
Anticonvulsant medication is the first line of treatment for patients with trigeminal neuralgia (TN). Neurosurgical treatment is reserved for those patients who fail to respond to medications or develop unacceptable medication side effects.
Neurosurgery treatment options for Trigeminal Neuralgia
Neurosurgical intervention is recommended when medication is not effective or medication side effects become unacceptable. Neurosurgical options include percutaneous “needle” procedures, Gamma Knife Radiosurgery (GKRS) and open skull surgery for Microvascular Decompression (MVD). Percutaneous needle procedures (balloon compression) and GKRS are both destructive procedures, performed on an outpatient basis, and are expected to cause some facial numbness. The amount of numbness is usually mild and willingly accepted by most patients in place of the severe TN pain. Although MVD is the most invasive and complex procedure performed for patients with TN, it is also the most effective procedure for TN and the only surgical procedure that spares the trigeminal nerve. Below are some of the surgical methods we use to treat intractable TN.
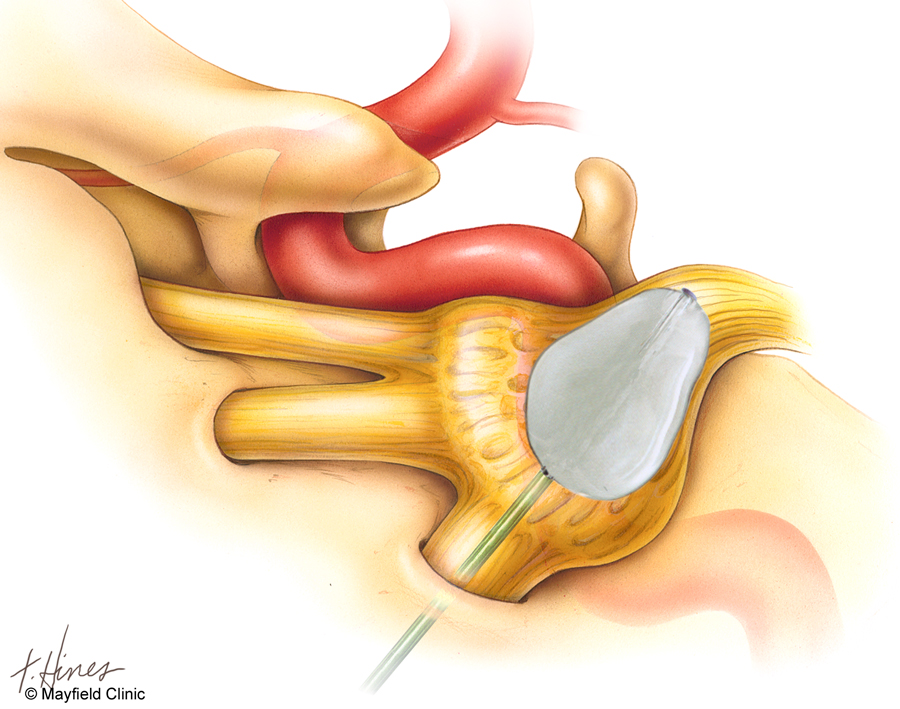
Percutaneous Balloon Compression
Percutaneous Balloon Compression is a safe and effective out-patient procedure, which provides rapid relief of severe pain in most patients, with minimal risk and early recovery. Following general anesthesia, a needle is passed through the cheek and directed to the skull base. A small balloon tipped catheter is passed through the needle and positioned against the nerve and inflated in order to compress the nerve and cause just enough injury to relieve the Trigeminal Neuralgia pain.
Relief of severe TN pain is usually immediate, but occasionally can take up to 24-48 hours. Patients can resume activities without restrictions the day following the procedure. Some numbness is expected after compressing the nerve and correlates with better long term pain relief. If patients still have pain after 24 hrs, the procedure is repeated using a longer compression time. There is an approximately 85-90% initial success rate after PBC. Patients with multiple sclerosis (MS) have higher rates of recurrence. Symptoms can gradually return over time, with a five-year recurrence of around 50%.
Gamma Knife Radiosurgery
Gamma Knife Radiosurgery is an out-patient procedure which does not require general anesthesia. On the day of treatment a head frame is applied utilizing a local anesthetic and brief moderate sedation An MRI scan of the brain is then obtained and the images are transferred to the Gamma Plan workstation. The trigeminal nerve is identified and targeted to receive a highly focused dose of radiation while sparing the surrounding structures in the brain from any harmful radiation. Patients may return home on the day of the procedure after a short period of observation. Restrictions on activities after Gamma Knife radiosurgery are not necessary and patients may resume pre-admission activities without delay.
Since it takes about 4-6 weeks, on average, to get relief of pain, we recommend that patients continue to take their trigeminal neuralgia medication until symptoms improve. Patients who have more constant and aching pain patients with multiple sclerosis are less likely to achieve lasting pain relief following GK, as is the case for any neurosurgical intervention for TN.
About 70% of patients reportsignificant pain relief (no pain, occasional pain not requiring medication or some pain adequately controlled with medication) at one year after treatment. Pain relief may gradually decrease overtime with about 50% of patients reporting significant pain relief at five years..
General Anesthesia
The patient is given general anesthesia. Their head is fixed in a device that keeps the head in position during surgery.
Initial Incision
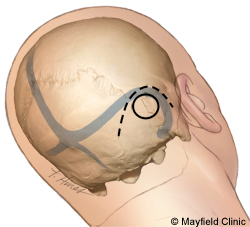
A small incision is made in the skin behind the ear. The skin is moved aside and an opening is made in the skull. The surgeon removes the bone to expose dura (the protective covering of the brain). An incision is made in the dura, which allows access to the brain.
Move Tissues
The brain is gently moved (retracted) until the surgeon has access to cranial nerves and surrounding blood vessels.
Separate Blood Vessels
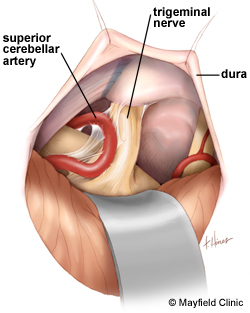
Next, the trigeminal nerve is carefully inspected, looking for the offending vessel (artery or vein) that is causing pathological compression of the nerve. The artery is carefully mobilized away from the nerve and various techniques, including using a small piece of shredded Teflon felt material, may be used to reposition the artery away from the nerve. A video of the MVD procedure can be viewed on this website page.
Dura Replaced
The dura is replaced and sealed. The bone is replaced or bone substitute may be used. The whole procedure takes two to three hours.
Potential risks and complications include infection, spinal fluid leakage, cranial nerve injury and stroke with an overall complication rate of less than a few percent.
What happens after Microvascular Decompression Surgery?
After the procedure, we transfer the patient to ICU for close monitoring. The patient may experience nausea which we can control with medication.
Typically, within two to three days, the patient will be discharged from the hospital.
In most cases, the patient gets immediate facial pain relief. However, in a few cases they may experience some residual face pain symptoms for a few weeks. MVD is the most effective procedure available for Trigeminal Neuralgia and provides immediate relief in about 95% of patients. About 15% of patients will have pain recurrence within ten years.
There is no one procedure which is best for every patient with Trigeminal Neuralgia. Management options are thoroughly reviewed with every patient and treatment is individually tailored for each patient’s specific needs and circumstances.
This material is intended to give the patient an overview of surgical procedures and treatments and is not intended to replace the advice and guidance of a physician. Always consult with your doctor about the particular risks and benefits of your treatment.


 The Highest Quality of Neurosurgical Care
The Highest Quality of Neurosurgical Care